Living with amyotrophic lateral sclerosis (ALS) brings many physical changes over time.
ALS gradually affects a person’s ability to walk, use their hands, speak, and eventually breathe independently. While there is currently no cure, supportive care can help improve comfort, mobility, and quality of life.
Physical therapy is a key part of that support. It can help people with ALS stay active for as long as possible, reduce stiffness and discomfort, and support overall well-being. 1, 2, 3, 4, 5
This blog explores the role of physical therapy in ALS care, including exercises that can help maintain mobility, flexibility, and balance. It also provides an overview of techniques related to breathing support, as well as assistive devices and home modifications that are often referenced in discussions about supporting people with ALS with daily activities.
Amyotrophic lateral sclerosis (ALS) is a progressive neurological disorder that affects motor neurons. These are nerve cells in the brain and spinal cord responsible for controlling voluntary muscle movements, including the muscles involved in breathing. 6, 7
As these nerve cells gradually weaken and die, the muscles they control stop working properly. Muscle weakness increases over time, making movement more difficult and often leading to the need for breathing support in later stages.
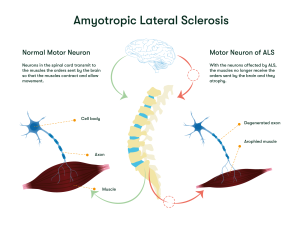
As ALS progresses and motor neurons deteriorate, the muscles they control become weaker, may twitch (called fasciculations), and start to shrink (known as atrophy). 6, 7
Symptoms vary from person to person, but common early signs of ALS include:
Later ALS symptoms may include:
In advanced stages, people with ALS may lose the ability to stand, walk or move their hands and arms. They may also need support to breathe. Since they typically retain the capacity to reason, remember, and understand, they are aware of their gradual loss of function. For both the person living with ALS and their loved ones, this can cause anxiety or depression.

In this blog, we focus on how physical therapy can support people living with ALS. For more information about ALS symptoms, risk factors, diagnosis, and treatment, you can explore our dedicated blog.
Physical therapy (also known as physiotherapy) is a form of care that helps maintain or improve a person’s ability to move and do everyday activities. It is often recommended when a disease, injury, or disability limits normal movement. Physical therapy is performed by a health care professional called a physical therapist.
Because ALS is a progressive and debilitating condition that affects every person with ALS differently, therapy plans are personalized and adjusted over time as needs change. Programs may include a combination of movement exercises, breathing training and massages. Therapists may also recommend assistive devices and home modifications to make daily life easier.
For people with ALS, the role of physical therapy is not to rebuild lost muscle, but to help:
In the following sections, we’ll describe different types of exercises that may be relevant to mobility, flexibility, balance, and breathing. We’ll also outline techniques and equipment commonly used to support safety and comfort in daily activities for people living with ALS. As experiences with ALS vary between individuals, the relevance of these approaches may differ; you may wish to discuss which options, if any, are appropriate for you with your medical team.
Mobility exercises can help people with ALS stay as active and independent as possible. They are best guided by a physical therapist and adapted to each person’s needs. They may include a combination of stretching and range-of-motion (ROM) exercises, light resistance training, low-impact aerobic activity, and simple balance exercises. Each type of exercise has a different purpose, and together they can help support safe movement and overall well-being.
Stretching and range-of-motion (ROM) exercises are gentle movements that help keep muscles flexible and joints moving comfortably.
These exercises are often performed together in daily routines. Common examples of stretching and ROM exercises include:
Stretching and ROM exercises are intended to be gentle and performed without forcing any movement. Motions can be kept slow and paused immediately if there is pain, discomfort, or unusual fatigue. This is especially important because overexertion may lead to soreness or injury. 12
Light resistance exercises can help people with ALS maintain their existing muscle strength for as long as possible. Unlike traditional strength training, the goal is not to build new muscle. Instead, the aim is to keep the muscles that are still working active without causing fatigue or injury. 1, 4 These exercises are usually most appropriate in the early stages of ALS, when some muscles can still move comfortably.
These activities may use simple tools, such as:
People with ALS are often advised to use very light resistance and repeat each movement several times, especially with muscles that can still move well. Using slow and steady movements can help lower the risk of injury.4 The exercises can be paused or adjusted if fatigue, cramping, twitching, or soreness appear, as it may be a sign of overwork.1
Aerobic exercise involves rhythmic, repetitive muscle movements that increase heart rate and oxygen use. Low-impact aerobic activity involves these same principles but is performed gently, placing minimal stress on the joints and muscles. 13, 14
For people living with ALS, low-impact aerobic exercises may help support heart and lung health, keep unaffected muscles strong, improve circulation, and reduce tightness.1, 2, 4, 15 Common examples include:
Many people with ALS find pool exercises helpful because the water supports the body. This makes movement easier and lowers the risk of falling.2
Activities like walking, cycling, swimming, and aquatic therapy can help keep the heart and lungs working well, improve blood flow, and support overall health. But because breathing muscles can get weaker over time, high-intensity cardio that causes shortness of breath is usually not recommended. More intense workouts can put extra strain on the lungs and make fatigue worse. 4

As ALS progresses, weakness in the legs, trunk, or arms can affect balance and increase the risk of falls. Assistive devices often play an important role in staying safe in these cases. However, physical therapists may also recommend simple balance activities to help individuals remain as steady and secure as possible. These exercises are typically done with supervision and may be performed either standing or seated, depending on the person’s abilities.
Balance activities may include movements such as:
These exercises are usually practiced near a stable surface, such as a counter, wall, or sturdy chair, to allow for support if needed. The goal is not to demand too much from the body, but to maintain safe movement patterns, improve confidence, and reduce the risk of falls.1, 4
Massage therapy involves applying gentle pressure to the body’s soft tissues, including muscles, tendons or ligaments.
Massage is not intended to strengthen muscles or slow disease progression. However, it can help reduce stiffness, reduce discomfort, and promote relaxation. Many people also feel that massage improves circulation, lowers tension, and provides a sense of comfort and well-being. 5, 16, 17, 18

Breathing exercises can be an important part of physical therapy for people living with ALS. As breathing muscles become weaker, these exercises may help make breathing easier, support a stronger cough, and help clear mucus.
Common breathing techniques for ALS include:
As ALS progresses and breathing becomes harder, additional support may be needed. Two common options include:
These therapies can be adjusted over time to match an individual’s comfort, breathing strength, and stage of disease. As with physical therapy, respiratory techniques and devices should be selected by the individual’s treating healthcare team, including respiratory and physical therapists, based on each person’s specific needs, overall condition, and stage of ALS. The healthcare team can also help determine how to safely incorporate these approaches into daily care.
As ALS progresses, many individuals benefit from assistive devices that support mobility, safety and comfort. A physical or occupational therapist can help determine which devices are most appropriate at each stage.
Common types of assistive devices include:

In addition to mobility devices, changes to the home environment can help individuals with ALS move more safely and manage daily activities. Physical and occupational therapists often recommend these adaptations based on the person’s abilities, goals, and daily routines and stage of ALS. 2, 20, 21
Common home modifications may include:

Living with amyotrophic lateral sclerosis (ALS) involves ongoing physical and functional changes that can affect many aspects of daily life. Although there is no cure, a range of supportive strategies can play an important role in helping people adapt to these changes and improve comfort, safety, and quality of life.
Physical therapy, also called physiotherapy, represents one part of this broader approach to ALS care. Through carefully selected exercises, breathing strategies, techniques, assistive devices, and home adaptations, physical therapy can help address mobility challenges, reduce discomfort, and support daily functioning. Importantly, these interventions are not one-size-fits-all and do not replace other aspects of care
ALS requires a multidisciplinary and individualized care plan, involving physical and respiratory therapists, physicians, and other healthcare professionals. Decisions about therapy and supportive tools should be adapted to each person’s abilities, symptoms, and stage of disease, and adjusted over time as needs evolve.
While this article focuses on physical therapy and supportive care in ALS, ongoing clinical research continues to explore potential approaches for understanding and managing the condition.
If you’re interested in learning about clinical trials related to ALS, you can book a call with a Patient Navigator.
At myTomorrows, we have a team of Patient Navigators, who are multi-lingual professionals with a medical background, who can support you with information and support at the different stages of the clinical trial process.
[1] M. Fox and K. K. Pt, “Exercise with Amyotrophic Lateral Sclerosis (ALS) Produced by Fact Sheet”, doi: 10.1097/PHM.0000000000001419.
[2] ALS Association, “Mobility and ALS.” Accessed: Nov. 21, 2025. [Online]. Available: https://www.als.org/navigating-als/living-with-als/therapies-care/mobility-als
[3] V. D. Bello-Haas, “Physical therapy for individuals with amyotrophic lateral sclerosis: current insights,” Degener Neurol Neuromuscul Dis, vol. 8, p. 45, Jul. 2018, doi: 10.2147/DNND.S146949.
[4] Your ALS Guide, “Exercise and ALS.” Accessed: Nov. 21, 2025. [Online]. Available: https://www.youralsguide.com/exercise-and-als.html
[5] American CPR Care Association, “Effective Therapies for ALS: Enhancing Quality of Life for Patients.” Accessed: Nov. 25, 2025. [Online]. Available: https://cprcare.com/blog/therapies-for-als/
[6] Mayo Clinic, “Amyotrophic lateral sclerosis (ALS).” Accessed: Nov. 26, 2024. [Online]. Available: https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022
[7] National Institute of Neurological Disorders and Stroke, “Amyotrophic Lateral Sclerosis (ALS).” Accessed: Dec. 03, 2025. [Online]. Available: https://www.ninds.nih.gov/health-information/disorders/amyotrophic-lateral-sclerosis-als
[8] Merriam Webster, “PHYSICAL THERAPY Definition & Meaning – Merriam-Webster.” Accessed: Nov. 20, 2025. [Online]. Available: https://www.merriam-webster.com/dictionary/physical%20therapy
[9] Timothy Gower, “What Is Physical Therapy?” Accessed: Nov. 20, 2025. [Online]. Available: https://www.webmd.com/pain-management/what-is-physical-therapy
[10] Institute for Quality and Efficiency in Health Care (IQWiG), “In brief: Physical therapy,” Mar. 2024, Accessed: Nov. 20, 2025. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK561514/
[11] Cleveland Clinic, “Physical Therapy (Physiotherapy): What It Is & Benefits.” Accessed: Nov. 20, 2025. [Online]. Available: https://my.clevelandclinic.org/health/treatments/physical-therapy
[12] ALS Network, “ALS Range of Motion Exercises.” Accessed: Nov. 21, 2025. [Online]. Available: https://alsnetwork.org/navigating-als/living-with-als/resource-guides-for-daily-living/als-home-and-daily-living-guide/als-range-of-motion-exercises/
[13] Cleveland Clinic, “Aerobic Exercise: What It Is, Benefits & Examples.” Accessed: Dec. 01, 2025. [Online]. Available: https://my.clevelandclinic.org/health/articles/7050-aerobic-exercise
[14] Cleveland Clinic, “7 Low-Impact Cardio Exercises To Try.” Accessed: Dec. 01, 2025. [Online]. Available: https://health.clevelandclinic.org/low-impact-cardio
[15] Physiopedia, “Amyotrophic Lateral Sclerosis.” Accessed: Nov. 21, 2025. [Online]. Available: https://www.physio-pedia.com/Amyotrophic_Lateral_Sclerosis
[16] K. Blatzheim, “Interdisciplinary palliative care, including massage, in treatment of amyotrophic lateral sclerosis,” J Bodyw Mov Ther, vol. 13, no. 4, pp. 328–335, Oct. 2009, doi: 10.1016/j.jbmt.2008.04.040.
[17] ALS News Today, “Discovering the Benefits of Massage.” Accessed: Nov. 25, 2025. [Online]. Available: https://alsnewstoday.com/columns/discovering-benefits-massage/
[18] Amyotrophic Lateral Sclerosis Association of Canada, “Complementary Therapies. Fact sheet.” Accessed: Nov. 25, 2025. [Online]. Available: https://www.alsbc.ca/wp-content/uploads/2018/06/ALSCAN-Complementary-Therapies-EN.pdf
[19] ALS Network, “ALS Respiratory Support.” Accessed: Nov. 25, 2025. [Online]. Available: https://alsnetwork.org/navigating-als/living-with-als/resource-guides-for-daily-living/als-respiratory-guide/als-respiratory-support/
[20]Your ALS Guide, “ALS Equipment Guide.” Accessed: Nov. 25, 2025. [Online]. Available: https://www.youralsguide.com/als-equipment-guide.html
[21] The ALS Association, “Assistive Technology.” Accessed: Nov. 21, 2025. [Online]. Available: https://www.als.org/navigating-als/living-with-als/therapies-care/assistive-technology
About the author
Medical Content Writer at myTomorrows
Dr. Andrea Enguita Marruedo holds a master’s in Genetics and Cell Biology from the Autonomous University of Madrid and a PhD in Developmental Biology from the Erasmus Medical Centre in Rotterdam. She began her career in medical writing after completing her doctoral studies and has covered a wide range of therapeutic areas, including neuromuscular and neurodegenerative disorders, cancer, and diabetes.
Andrea specializes in translating complex biomedical topics into clear, accessible content for patients and healthcare professionals. With a strong research background and a passion for science communication, she is committed to delivering accurate, well-referenced content that supports greater awareness and understanding of medical topics among patients, caregivers, and clinicians.
Andrea Enguita 14 Jan 2026