This blog is designed to provide information about Amyotrophic lateral sclerosis (ALS) for those living with this condition, their caregivers, loved ones, and anyone interested in learning about this disease. Here, you’ll find information about what ALS is, how it is diagnosed, the symptoms, and both current and investigational treatments.
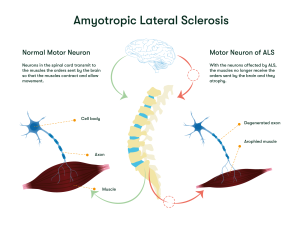
Amyotrophic lateral sclerosis (ALS) is a neurological disorder that impacts motor neurons — the nerve cells in the brain and spinal cord responsible for controlling voluntary muscle movements and breathing.1, 2 Over time, the disease leads to a loss of these functions, causing people with ALS to gradually become unable to do everyday activities like walking, talking, eating, and eventually breathing on their own.1, 2
ALS is a rare condition that affects 1.5 to 3 per 100,000 individuals every year in North American and European populations.3 Estimates of how common ALS is, suggest that approximately 30,000 people in the United States are living with the condition, with around 5,000 new cases diagnosed each year. The condition is slightly more common in men than in women overall, with about 60% of cases occurring in men. However, this difference changes with age. Before age 65, men are more likely to develop ALS than women, but after age 70, men and women are equally likely to be diagnosed with the disease. 1, 2, 3
It is believed that damage to motor neurons, which causes ALS, happens due to several interconnected bodily processes that cause widespread neuron damage. Some of these processes include:
Additional factors that may drive the disease include DNA damage, alterations in the transport of nutrients, waste, and signals within neurons, and damage to mitochondria, the tiny structures that provide energy to the cell to function. 5, 6
Most cases of ALS are classified as sporadic, meaning the disease appears to arise randomly, without any identifiable risk factors or a family history of the condition. 1, 2 However, about 10% of cases have a genetic basis (known as familial ALS) and are associated with mutations (changes in the DNA) that increase the likelihood of developing the condition.1, 2 Researchers have identified several mutations in different genes that can lead to familial ALS. For example, about 25-40% of all familial cases are caused by a mutation in the C9orf72 gene, while another 12-20% of familial cases result from mutations in the SOD1 gene. 1, 2
These mutations are inherited, meaning they are passed down from a parent. Our genes come in pairs—one copy from each parent. For most cases of familial ALS, the condition is inherited in an autosomal dominant pattern. This means a person only needs one copy of the mutated gene (from either parent) to have an increased risk of developing ALS. However, some less frequent forms of ALS are inherited in an autosomal recessive way, meaning a person must inherit two copies of the mutated gene (one from each parent) to develop the condition.8
Besides genetic factors, certain conditions are linked to a higher risk of developing ALS. These include being between 55 and 75 years old, being male, and being White or non-Hispanic.1, 2 Environmental factors, such as smoking or exposure to toxins are also associated with a higher risk of developing the disease. Interestingly, some studies suggest that people who have served in the military are also at higher risk of developing ALS. Although it is unclear what aspects of military service may trigger ALS, potential factors include exposure to specific metals or chemicals, traumatic injuries, viral infections, or extreme physical exertion. 1, 2, 9 However, it is important to note that having these risk factors does not mean a person will develop ALS, and people without risk factors can still develop the disease. 1, 2
In ALS, motor neurons gradually stop working properly and eventually die. When this happens, the muscles they control become weaker, may twitch (a symptom called fasciculations), and shrink (known as atrophy).1,2
Some early signs of ALS may include muscle cramps in the arm, leg, shoulder, or tongue, trouble walking, tripping and falling, weakness in the legs, arm or neck, slurred and nasal speech and tight and stiff muscles (spasticity). Later, ALS symptoms may include trouble chewing food and swallowing (dysphagia), unintentionally loss of saliva from the mouth (drooling or sialorrhea), trouble speaking or forming words, unintended crying, laughing, or other emotional displays, constipation and trouble breathing (dyspnea).1, 2
In advanced stages, people with ALS may lose the ability to stand, walk, independently get in and out of bed, use their hands and arms, or breathe without assistance. Since they typically retain the capacity to reason, remember, and understand, they are aware of their gradual loss of function. Understandably, this can cause anxiety and often depression for a person living with ALS, as well as potentially for their loved ones also.1
Diagnosing ALS can be challenging, particularly in the early stages, as its symptoms often resemble other conditions.1, 2 To confirm an ALS diagnosis and rule out other diseases, healthcare professionals may use a combination of tests, including:

While there is no cure for this disease at the moment, some ALS treatments are available to help manage symptoms, slow down the disease and improve quality of life.
In the U.S., the ALS medications Riluzole (Rilutek), Edaravone (Radicava) or Tofersen (Qalsody) are approved by the Food and Drug Administration (FDA). 1, 10 In Europe, only Riluzole (Rilutek) and Tofersen (Qalsody) are approved by the European Medicine Agency (EMA). 11, 12 These drugs work in different ways to target specific aspects of the disease:
Another medicine, Relyvrio/Albrioza, was previously approved and used in the U.S. However, the manufacturer announced its removal from the market as of September 2024 after it did not meet the expected results in a phase 3 clinical trial. 18, 19
Besides medication, a treatment plan for ALS usually includes supportive care tailored to individual needs:
 Speech therapy can help maintain the ability to speak loud and clear.
Speech therapy can help maintain the ability to speak loud and clear.
Developing new treatments for ALS is challenging, partly because the disease varies so much between individuals. 20 Investigational treatments for ALS focus primarily on slowing disease progression, protecting motor neurons, and targeting specific mechanisms that drive the disease. Some of the treatments currently being explored in ALS clinical trials or preclinical studies include:
Small molecules are simple chemical substances that can easily enter the body’s cells due to their size, making them versatile tools for targeting various biological processes Different types of small molecules are being investigated in ALS clinical trials with the aim of targeting several key aspects involved in ALS, including:
By addressing these key processes, small molecules aim to slow down the progression of ALS and improve the symptoms of those affected.
Gene-specific therapies are designed for individuals with identified genetic mutations associated with ALS and are not intended for cases of sporadic ALS. In these individuals, specific mutations can lead to the production of harmful proteins that damage motor neurons and contribute to disease progression.
One of these genetic-specific approaches involves the use of antisense oligonucleotides (ASOs), synthetic molecules that block the formation of these harmful proteins with the objective of protecting motor neurons from damage. The first approved ASO is the medicine Tofersen, specially designed for people with an ALS SOD1 mutation. Other ASOs are being studied in clinical trials for different mutations.21, 22
Immunotherapy involves the treatment of a disease by stimulating or suppressing an immune response. In ALS, one form of immunotherapy involves the use of antibodies, which are special proteins designed to target and block harmful substances in the body. Researchers are exploring whether antibodies and other immunotherapies could slow disease progression by reducing inflammation, restoring the balance of certain proteins that protect nerve cells, or addressing specific genetic factors associated with ALS. These investigational therapies are currently being tested in ALS clinical trials. 20, 21, 22
Stem cells are special cells in the body that can transform into different types of cells, such as muscle cells or brain cells, depending on where they are in the body and the signals they receive. These qualities make them of interest for researchers to treat different types of conditions.23 In the field of ALS, researchers are exploring how stem cells might be used to generate healthy neurons to replace those damaged or destroyed by the disease. This investigational ALS treatment is currently being studied in clinical trials.20, 21
Amyotrophic lateral sclerosis (ALS) is a neurological disorder that affects motor neurons, which gradually stop working properly and eventually die within the body. This leads to a progressive loss of the ability to control movements like walking, talking, chewing, and breathing. While there is no cure, various ALS treatments can help manage symptoms and improve the quality of life. The physician might indicate treatment with the medications Riluzole, Tofersen or Edaravone (only in the U.S.), and supportive treatment such as physical, occupational and speech therapy. There are several investigational treatments for ALS being explored in clinical trials, including the use of small molecules, gene-specific therapies, immunotherapy and stem cells.
If you are affected by ALS and want to explore clinical trial options, you can book a call with a Patient Navigator to discuss your options and learn more about participating in clinical trials.
At myTomorrows, we have a team of Patient Navigators, who are multi-lingual professionals with a medical background, who can help you to explore your treatment options and support you through your journey.
myTomorrows Team 11 Feb 2025